Heart hypertrophy
After a recent historical silver in Russia “Vatreni” are under increased attention of media, so not a day goes by without some news of Zlatko Dalic’s chosen. Although there are usually speculations about transfers and earnings, this time there have been some unfortunate medical news. The last that flooded the social networks concerned the public with the diagnosis of the initial stage of heart hypertrophy of the left AC Milan defender – Ivan Strinić. Given that it is nonetheless the heart in question, the drama is not lacking, and the media does not save words for it so the British The Sun writes: “HEARTBREAKER World Cup finalist Ivan Strinić puts career on hold after shocking heart problem revealed” (1). On the other hand, for big Croatian journal “Slobodna Dalmacija”, Strinić calmly explains that doctors are just cautious but there is no reason to be worried because athlete’s heart is usually bigger than normal.
Since such medical diagnosis brings a lot of attention and confusion in general public, I have decided that it would not be in vain writing about secrets of athlete’s heart.
Let’s start at the beginning. Why is there a heart hypertrophy?
For the purposes of this article, imagine a muscle cell. To function normally this cell needs oxygen, nutrients and constant drainage of carbon dioxide and harmful substances. Cardiovascular system effortlessly takes care of those if two conditions are met: 1) oxygen and nutrients can be transported through blood and 2) enough blood comes to the cell. At a time when our imaginary muscle cell works particularly intensely (for example during endurance training) the need for oxygen and nutrients is increased. For the cardiovascular system to continue to satisfy the needs of the cell it needs to: 1) transport more oxygen and nutrients in the same volume of blood or 2) enable the flow of an even larger volume of blood to the cell. Studies show that the body decides for option 2. The primary adaptation to endurance training is the delivery of larger volumes of oxygenated blood to muscle cells, which is achieved by increased heart rate. Medical dictionary would say that the cardiac volume increases, i.e. the volume of blood ejected by the heart in one minute. Cardiac output is the product of the heart rate and the volume of blood that is eject during one contraction (stroke volume). Given that a large increase in the heart rate reduces the time of filling of the heart with blood, adaptation of the heart to endurance training is an increase in the volume of blood that the heart can eject with any contraction. For easier understanding, Figure 1. shows the values of cardiac minute volume (SMV), impact volume and maximum heart rate (HR) are presented for inactive persons, recreational and top athletes in endurance sports. Based on the data shown, it is obvious that adaptation to endurance training in athletes and amateurs is based primarily on the increase of stroke volume.
* Short digression *
Interestingly, based on the data shown, it turns out that the training of endurance reduces the maximum heart rate which is still the subject of debate among researchers (e.g., see Zavorsky (2000) 3), but keep this for another blog :D.
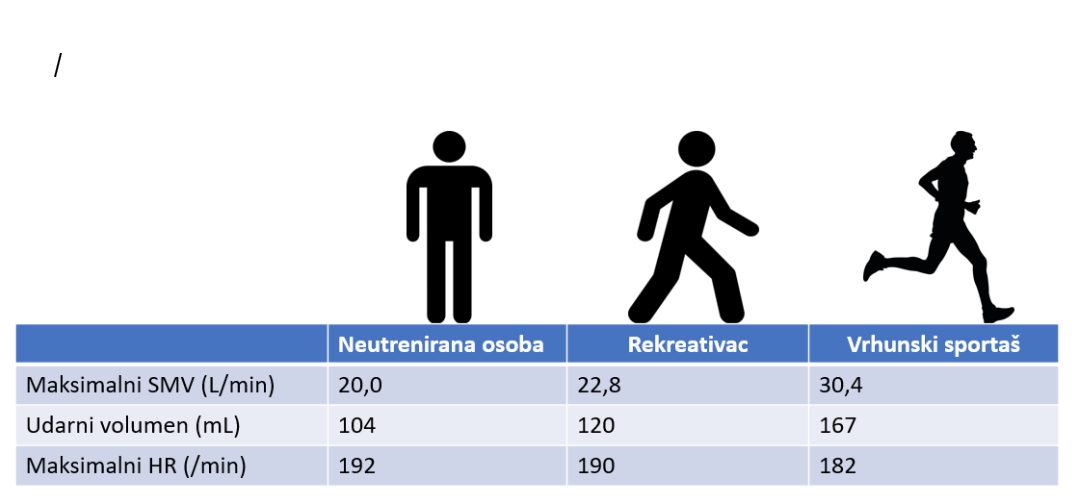
Figure 1.
Values of the maximum cardiac output, stroke volume and maximum heart rate in individuals with varying levels of physical activity. SMV – cardiac output; HR – heart rate. (4,5).
It remains to answer the question on what happens to the heart that enables achieving such high values of stroke volume?
You’re right! – exercise triggered the heart muscle hypertrophy and that is known as the “Athlete’s heart” (remember again Strinić’s comment for “Slobodna Dalmacija”). More precisely, the athlete’s heart is characterized by increased left ventricular volume and mild thickening of the heart muscle, which makes the heart in athletes often larger and heavier than the average (4). Guyton, for example, states that the marathoner ventricles were increased by approximately 40%, which corresponds to a 40% increase in heart mass (6). However, heart muscle hypertrophy is not only occurring in athletes, so it is necessary to differentiate the physiological hypertrophy (an athlete’s heart) from the pathologic.
As opposed to physiological hypertrophy, the pathological hypertrophy of the heart muscle is characterized by a significant thickening of the ventricular walls with a buildup of non-contractile proteins, which has functional consequences (4). In the athlete’s heart the ejection fraction (percentage of total volume of blood ejected in a single contraction) is preserved while in the pathologic hypertrophy is decreased. In other words, heart is hypertrophic in both cases but in physiological hypertrophy strength increases proportionally with size while in pathological it decreases. Pathological hypertrophy manifests as chest pain, dyspnea, heart palpitations or syncope in exercise, and those symptoms should be taken seriously. With respect to clinical examination results and described symptoms it is possible to suspect the existence of pathological hypertrophy which can be confirmed by electrocardiography, ultrasound and exercise testing. Regular medical examinations of athletes are important for right diagnostics and differentiating potentially dangerous states.
And for nerds …. the background:
The moment it was discovered that two types of hypertrophy are different, the key question emerged whose answer was supposed to be given by molecular physiology. Are physiological and pathological hypertrophies connected on molecular level and what signal pathways underlie each? Results of many in vivo and in vitro research have given us part of the answer on this puzzle. It seems that there are different signal pathways for both hypertrophies (Picture 2.) (4,7). Pathological hypertrophy is connected to signal pathways regulated by intra and extracellular calcium (calmodulin, calcineurin), reactive oxygen species, some protein-kinases activated by mitogens and inflammation. On the other hand, physiological hypertrophy is mediated through signal pathways connected to mTOR system.
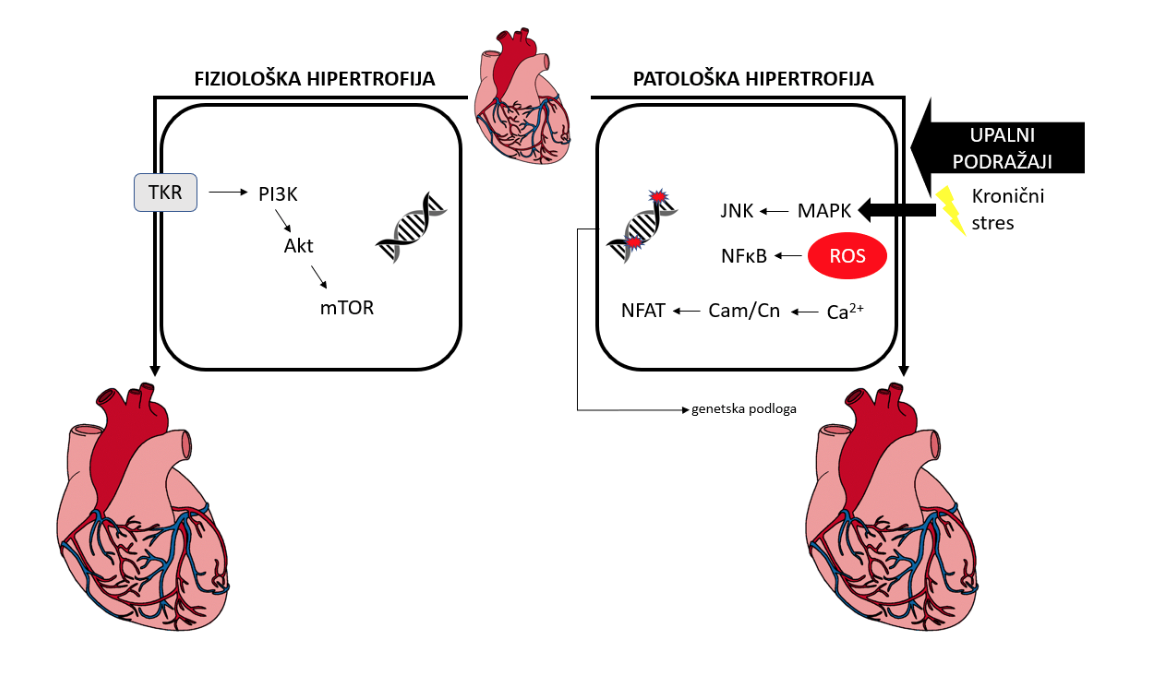
Picture 2. Main signal pathways in development of pathological and physiological hypertrophy of the heart. TKR – Tyrosine kinases receptor; PI3K – Phosphoinositide 3-kinase; mTOR – Mammalian target of rapamycin; NFAT – Nuclear factor of activated T-cells; Cam/Cn – calmodulin/calcineurin; ROS – reactive oxygen species; NFxB – nuclear factor kappa B; MAPK – mitogen activated protein kynases; JNK – c: c-Jun N-terminal kinases. (according to Sama et al., 2016) (7)
And finally…
Simplified signal pathways denoted on Picture 2. should illustrate the same very thing that inspired me for writing this blog. Albeit hypertrophy of heart muscle is still very unclear, it is evident that Athlete’s heart and Pathological heart are two different entities often pushed together into the same bucket. That happens because macroscopic difference is not always obvious. Despite that, molecular background and consequently functional outcomes are diametrically opposite. Albeit research on molecular background of this physiologic process will contribute to development of more precise diagnostics and therapy of heart hypertrophy, caution is still neded and one should never forget that things are not always black and white. There is no clear cut-off line like I showed you on picture 2. (you see those small red DNA explosions on the right illustration that represent genetical abnormalities considered to be common cause of death in athletes!).
References:
- Aasa, B., Berglund, L., Michaelson, P., & Aasa, U. (2015). Individualized Low-Load Motor Control Exercises and Education Versus a High-Load Lifting Exercise and Education to Improve Activity, Pain Intensity, and Physical Performance in Patients With Low Back Pain: A Randomized Controlled Trial. Journal of Orthopaedic & Sports Physical Therapy, 45(2), 77–85. http://doi.org/10.2519/jospt.2015.5021
- Erglund, L. A. R. S. B., Jo, B., & Asa, U. L. A. (2015). Which patients with low back pain benefit from deadlift training?, 29(7), 1803–1811.
- Kenney, W. L., Wilmore, J. H., & Costill, D. L. (2012). Physiology of sports and exercise.
- Lauersen, J. B., Bertelsen, D. M., & Andersen, L. B. (2014). The effectiveness of exercise interventions to prevent sports injuries: A systematic review and meta-analysis of randomised controlled trials. British Journal of Sports Medicine, 48(11), 871–877. http://doi.org/10.1136/bjsports-2013-092538
- Rønnestad, B. R., Nygaard, H., & Raastad, T. (2011). Physiological elevation of endogenous hormones results in superior strength training adaptation. European Journal of Applied Physiology, 111(9), 2249–2259. http://doi.org/10.1007/s00421-011-1860-0
- Skelton, D., & Beyer, N. (2003). Exercise and injury prevention in older people. Scandinavian Journal of Medicine & Science in Sports, 13(1), 77–85. http://doi.org/10.1034/j.1600-0838.2003.00300.x